Interventions for diabetes-associated morbidity
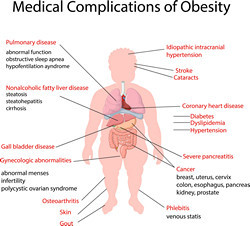
Europe alone spends billions of euros every year in the clinical management of metabolic disorders. The incidence of diabetes is estimated to rise by 20 % by 2030 in Europe. One of the most serious complications of diabetes and obesity is the liver condition known as non-alcoholic steatohepatitis (NASH), which is associated with steatosis and inflammation. The prevalence of NASH is high and ever increasing, not only in over-weight children and adults but also in insulin-resistant individuals of normal weight. The benign condition that precedes NASH is termed non-alcoholic fatty liver disease (NAFLD) where inflammation leads to fibrosis, cirrhosis and eventually liver failure. Although our understanding of the disease mechanisms has progressed, the therapeutic options for NASH remain poor. Scientists on the EU-funded MANASH (Exploiting the MSP-AMPK pathway for amelioration of NASH) project set out to develop novel therapeutic options for NASH. Research activities focused on AMP-activated protein kinase (AMPK), an important integrator of signals managing energy balance. Scientific evidence supports a vital role for AMPK in the metabolism of carbohydrates and lipids as well as protein synthesis and cell growth. An additional function of AMPK entails the reduction of inflammation. As a result, the MANASH consortium proposed to activate liver AMPK as a new therapeutic option for the treatment of NASH. In metabolic syndrome, AMPK activity is down-regulated and, thus, attempts have focused on the development of direct pharmacological activators. MANASH focused on macrophage-stimulating protein (MSP), a serum factor secreted from liver cells that exhibits anti-inflammatory properties on macrophages via activation of AMPK signalling. Researchers observed that in primary hepatocytes, MSP treatment led to significant activation of AMPK signalling and the effect was sustained even in the presence of lipogenic or inflammatory stimuli. MSP also reduced production of pro-inflammatory cytokines and increased anti-inflammatory signals. When they treated macrophages previously exposed to NASH-mimicking stimuli, a significant reduction in pro-inflammatory gene expression was noted. Taken together, the findings of the MANASH study underscore a role for MSP as a therapeutic intervention for NASH. However, in vivo and long-term studies are required to substantiate the efficacy and safety of MSP in the clinic.