MRI fat imaging could help manage metabolic syndrome and osteoporosis
Biomarkers are well established for diagnosing metabolic syndrome(opens in new window), but interventions to prevent two of the most common outcomes – diabetes and cardiovascular complications – are ineffectual. While osteoporosis(opens in new window) is treatable with medication, early diagnosis is ineffective, with fracture risk poorly understood. What has recently linked understanding of these two diseases, is fat. “Probing fat’s properties at the cellular level could provide groundbreaking solutions which overcome existing challenges in preventing metabolic syndrome and early diagnosis of osteoporosis,” explains Dimitrios Karampinos from the Technical University of Munich(opens in new window) and ProFatMRI project coordinator. The project, funded by the European Research Council(opens in new window), adapted magnetic resonance imaging (MRI) to non-invasively assess, in a single examination, the microstructure of both bone marrow and adipose tissue(opens in new window), comprised mainly of fat cells.
More robust biomarkers
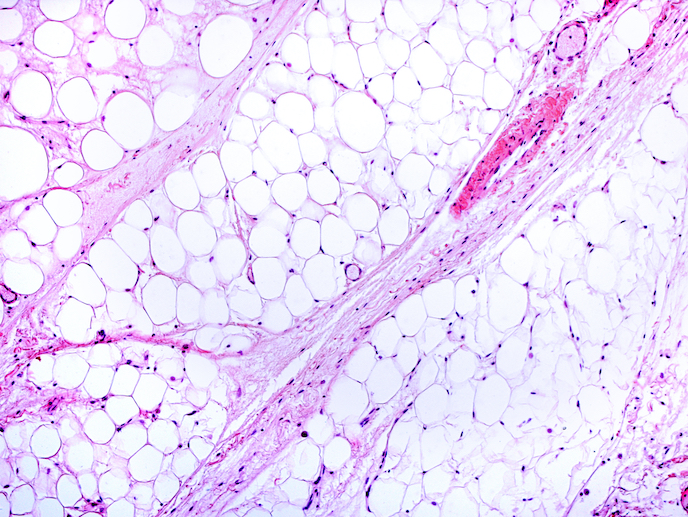
Current fat biomarkers for metabolic syndrome leave unanswered questions such as: why don’t all obese patients develop type 2 diabetes? Fat can be white or brown. White fat stores excess energy, whereas brown fat converts energy into heat. Excessive white fat is characteristic of obesity, and large white fat cells have been linked to insulin resistance. Recent evidence suggests that brown fat helps prevent metabolic syndrome. Being able to measure the volume and microstructure of both fat types could yield useful clinical information. The traditional diagnostic biomarker for osteoporosis is bone mineral density (BMD). But this has proven inadequate for identifying fracture risk. Even with high BMD, type 2 diabetics are at increased risk of fracture. Recent evidence suggests that higher marrow fat content correlates with fracture risk.
The imaging breakthrough
ProFatMRI set out to non-invasively differentiate white and brown fat and characterise bone mineral content and bone marrow. The team first had to develop data acquisition and processing methods so that MRI could focus on the protons of fat molecules, rather than of water. Tissue fat content and other properties were then imaged to differentiate white from brown. “We showed that the difference in the tissue fat content between a typical white fat region and a typical brown fat region in humans is linked to cold-induced heat production. Put simply, people who produce more heat in response to cold are expected to have higher amounts of brown fat, suggesting a potentially healthier metabolism,” adds Karampinos. The team also developed novel MRI methods to non-invasively measure human lipid droplet size, to gauge white fat cell size. These measurements were validated against samples under a microscope. The MRI techniques were also used to assess bone marrow fat and the thin cortical bone in the spine, where fractures typically occur. “We are the first to use radiation-free CT-like MR imaging techniques in patient studies to simultaneously measure bone marrow and cortical bone tissue changes,” says Karampinos. The marrow fat was shown to differ depending on the age and sex of subjects, unlike the bone, suggesting complex pathophysiological influences on fat cells. These findings were validated against computed tomography(opens in new window).
Towards the clinic
ProFatMRI’s techniques contribute directly to EU policies for obesity prevention and osteoporosis screening, outlined within the European Commission’s Health Promotion and Disease Prevention Knowledge Gateway(opens in new window). Under the FatVirtualBiopsy project, the team are currently developing a proof of concept that translates lipid droplet size measurements into a non-invasive tool to measure the size of human fat cells in vivo. They are also translating their bone and bone marrow imaging techniques into clinical spine examinations, especially to assess fracture in patients with degenerative spine changes and bone metastases.