Ultrasound contrast agents offer more precise radiotherapy
Around 50 % of cancer patients receive radiotherapy(opens in new window), which is constantly improving, precisely targeting tumorous cells with high radiation doses while protecting healthy cells. However, dosimetry, which ensures safety by verifying doses have reached the intended target, is lagging behind. “Currently, radiotherapy is like a road trip where the route is meticulously planned and the car equipped with high-tech navigation devices, but because the car’s windows are opaque it’s impossible to determine traffic conditions,” says Jan D’hooge, coordinator of the EU-supported AMPHORA project. To enhance patient safety, AMPHORA was set up to offer solutions for radiotherapy dose verification. The project developed a non-invasive technique to provide real-time assessments of radiation doses by casting ultrasound contrast agents into dose sensing theranostic devices(opens in new window). “By offering clinicians a way to verify dose distribution in the patient, our technology could revolutionise quality assurance and treatment follow-up,” explains Mihnea Vlad Turcanu, AMPHORA researcher.
Real-time irradiation imaging
Research previously conducted in KU Leuven’s(opens in new window) lab had revealed that certain contrast agents are sensitive to irradiation, offering a means to identify areas exposed to irradiation. AMPHORA’s principal aim was to optimise these agents, along with the process involved in quantifying the amount of irradiation reaching the target. The team experimented with a range of contrast agents comprising different chemistries, finding the most suitable type of nanodroplets. These have a liquid core and a shell composed of a water-soluble synthetic polymer. “Interestingly, nanodroplets are invisible on ultrasound images, but vaporise when exposed to radiotherapy; this transition to a gaseous bubble can easily be visualised on an ultrasound image by the appearance of a tiny bright dot,” adds Turcanu from KU Leuven, the project host.
The verification protocol
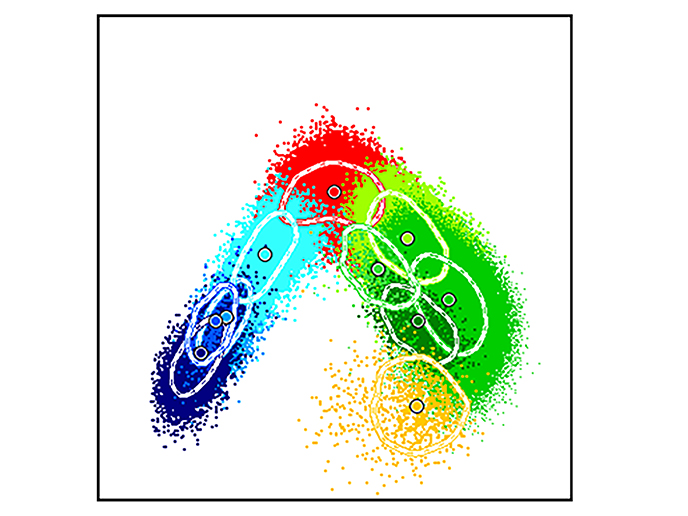
The contrast agents are injected into patients intravenously, where they accumulate in and around tumours. The vaporisation of these agents is then detected by an ultrasound probe. After experimenting with various designs, the team found a spiral probe worked best. The ultrasound imaging system, supported by a neural network called BubbleNet(opens in new window) – also custom-made by AMPHORA – overlays the vaporisation distribution on ultrasound images of the patient’s anatomy. Viewable on a screen by clinicians, this helps them see where, and in what quantities, irradiation is being delivered. “This reveals if healthy, as well as diseased tissue, is being irradiated, and if the correct dose is reaching the tumour, giving clinicians valuable real-time decision-making information about whether they need to adapt the therapy,” remarks Turcanu. A significant challenge was reaching the optimal radiation response, as the contrast agents required temperatures of around 50 °C, 13 °C higher than body temperature, for best performance. Not only was this technically complicated to achieve, it was unsafe for patients. The solution involved using an acoustic field which regulates pressure in the locality of interest, decreasing the sensitisation threshold of the contrast agents.
Commercial spin-off opportunities
AMPHORA’s proof of concept was successfully tested in phantoms(opens in new window) and live rats. Before making the device widely commercially available, possibly creating a spin-off company, the team will finalise testing on small animals then larger ones, before progressing to clinical trials. The project has already received letters of interest from key companies. “AMPHORA could trigger more novel technologies for radiation therapy and pave the way for other in vivo contrast agent-based sensing and therapeutic applications, such as targeted chemotherapy. This could help reduce the side effects of chemotherapy, while improving patient prognosis through increased synergy between chemotherapy and radiotherapy,” concludes Turcanu.