Human cartilage in a dish
The bones in our joints are lined with a smooth covering known as articular cartilage(opens in new window), which facilitates frictionless joint movement. It mainly consists of a collagen and glycosaminoglycan-rich extracellular matrix, generated by specialised cells known as chondrocytes. Articular cartilage cannot self-repair as it lacks blood vessels and a nerve supply. Therefore, damage or age-related degeneration may cause inflammation, pain and stiffness that may ultimately lead to osteoarthritis.
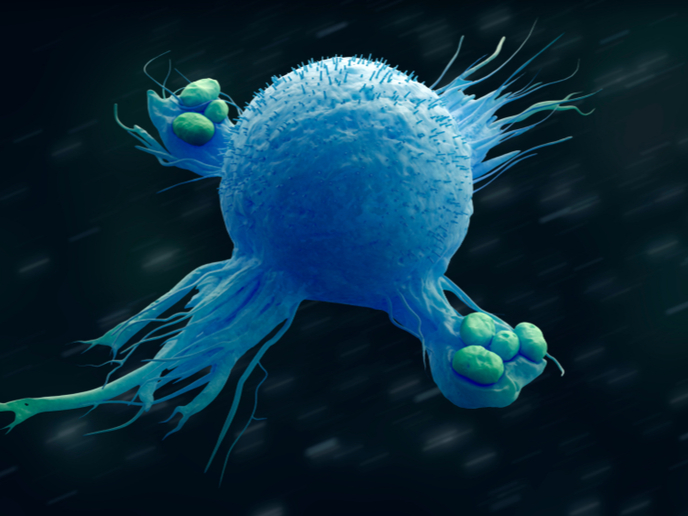
In vitro model of articular cartilage
Early treatment of articular cartilage damage may correct disease progression. However, suitable treatments remain inadequate due to gaps in our knowledge of how this type of cartilage forms in humans during development. To address this limitation, the ReSurface project developed methods to generate and study articular cartilage in the lab. The research was undertaken with the support of the Marie Skłodowska-Curie Actions(opens in new window) (MSCA) programme and involved an in vitro model that facilitates the investigation of early human cartilage development. “Previously, cartilage biology was studied using animal models. So, for the first time, our in vitro model pushes the frontiers of human cartilage biology. It will have an impact on developmental biology and cartilage disease research,” explains MSCA research fellow Rosanne Raftery.
From stem cells to cartilage
Researchers developed a method for generating stable articular cartilage tissue in a dish using human pluripotent stem cells(opens in new window) (hPSCs). This model enabled them to study human cartilage development for the first time, gaining a deeper understanding of how the cells produce cartilage tissue and how they respond to injury or ageing. Unlike adult articular chondrocytes, which lose their ability to produce healthy articular cartilage when expanded, hPSC-derived articular chondrocytes can repeatedly produce healthy articular cartilage. They also maintain stable behaviour, unlike adult bone marrow-derived stem cells, which tend to initiate bone formation instead of cartilage. Researchers undertook an in-depth analysis of hPSCs during their differentiation into articular chondrocytes and continued to study cell behaviour over long-term experiments, focusing on the maintenance of healthy cartilage. As well as generating new insights into human cartilage development, this led to the identification of novel drug targets that could mitigate the progression of osteoarthritis.
In situ regeneration of damaged cartilage
Adult articular chondrocytes are used clinically to treat cartilage damage and adult stem cells have been used in more than 120 clinical trials for cartilage repair. “We envision that our hPSC-derived articular chondrocytes can also be utilised for cell therapy in the future,” emphasises Raftery. For this purpose, the team developed and optimised a hyaluronic-based hydrogel for the delivery of hPSC-derived articular chondrocytes. Apart from carrying cells, this device could be used for drug delivery to sites of articular damage to stimulate articular cartilage regeneration in situ. This could halt the progression of osteoarthritis without the need for joint replacement surgery. The successful treatment of articular cartilage defects will limit pain and suffering for patients with obvious socioeconomic benefits including reduced work absenteeism and improved healthy and active ageing.