Hypoxia and haematopoiesis
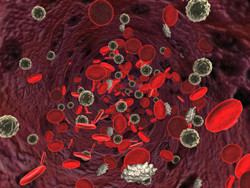
Like other tissue-specific stem cells, HSCs have the capacity to self-renew or differentiate into different blood cell types. Central to this decision is the bone marrow microenvironment and the cues it provides. Accumulating evidence indicates that HSCs are exposed to low oxygen levels in the bone marrow but the underlying molecular mechanisms have not been elucidated. With this in mind, scientists on the EU-funded 'The role of hypoxia-inducible factors in human haematopoietic stem cell biology and leukaemogenesis' (HSCS AND HIF) project decided to investigate the hypoxia-sensing system known as hypoxia inducible factor (HIF). Under normal oxygen levels, HIF has low transcriptional activity. However, at low oxygen levels, HIF regulates the transcription of crucial genes involved in cell proliferation, survival and differentiation. High HIF levels have also been reportedly found in various types of cancer and are associated with poor prognosis. Scientists looked at the levels of HIF factors in human HSCs and demonstrated their necessity for successful transplantation in a mouse model. Importantly, HIF2 affects the self-renewal of HSCs and their ability to maintain their stem-cell phenotype. Gene expression analysis of HSCs with reduced HIF levels underscored its importance in mitochondria homeostasis and reactive oxygen species production. Knockdown of HIF did not only make normal HSCs more prone to apoptosis but also impeded the growth of leukaemia cells. Collectively, the results of the HSCS AND HIF study provided the molecular link between the HSC phenotype and the hypoxic niche. The generated observations could have significant consequences for normal bone marrow transplantation. Results also offer a cue on how leukaemic cells evade chemotherapy and radiation.