New-generation joint replacement materials can prevent adverse immune reaction
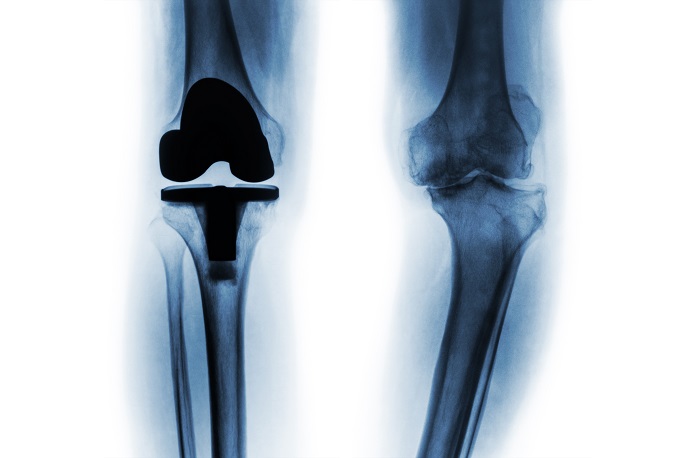
At first glance, the increasing success of orthopaedics that goes hand-in-hand with ever-aging populations is full of promises: instead of just living longer, we can now hope that this growing age won’t have too much impact on our lifestyles. Working a few more years, or enjoying retirement with a busy schedule is within reach. As Prof. Christoph Lohmann, coordinator of the HYPORTH (New approaches in the development of Hypoallergenic implant material in Orthopaedics: steps to personalised medicine) project on behalf of the University of Magdeburg, points out, joint replacements are particularly important to allow these dreams to come true. “Considering how most elderly people are living alone, sometimes far away from their family, mobility is getting more and more important. We are witnessing a greater demand for mobility and quality of life among elders, notably with regards to sports and other leisure activities, and joint replacements are the best available solution to meet such demand.” Joint replacements, however, don’t age too well. An increasing number of patients need to receive revision surgery due to complications, 10 % develop AIR to conventional implant material, and 10 % contract an infection. Not only can such periprosthetic infections not be avoided, but the numbers are constantly growing due to changing resistances and – to make things worse – no good predictive markers have yet been established to foresee such problems. “The main issue we face is loosening due to the likes of disintegration of prosthetic components, adverse reactions to biomaterials or malposition of implant, and infections which leave surgeons with no other choice but to revise or change prosthetic components. This problem is growing all over the world and represents a major burden for the patient and the health system in general,” says Prof Lohmann. This is the context in which the HYPORTH consortium was created. Over five years, the team led by Prof. Lohmann devised a predictive approach using biomarkers to identify patients at risk of developing AIR, and created new hypoallergenic material combinations for endoprostheses to avoid the immune reactions seen with conventional materials. The implant’s materials – hypoallergenic materials made of ceramics, polymers, pure titanium, or titanium particulate coatings that are wear resistant and biocompatible – can even be matched with the allergenic background of patients. As Prof. Lohmann points out, “implants may be individualised through production in certain 3D-print systems based to the anatomy of the patient and his/her potential allergies. Moreover, these implants can be equipped with sensors in order to early diagnose loosening.” Another important project outcome is the development of tests able to differentiate between AIR and septic loosening early. “Our prototypes will undergo clinical evaluation soon. Once it’s done, we will be planning for follow-up projects dealing with antibacterial surface modifications and sensors, as well as establishing new predictive and diagnostic biomarkers for better care,” Prof. Lohmann concludes.