Point-of-care test for meningococcal meningitis developed
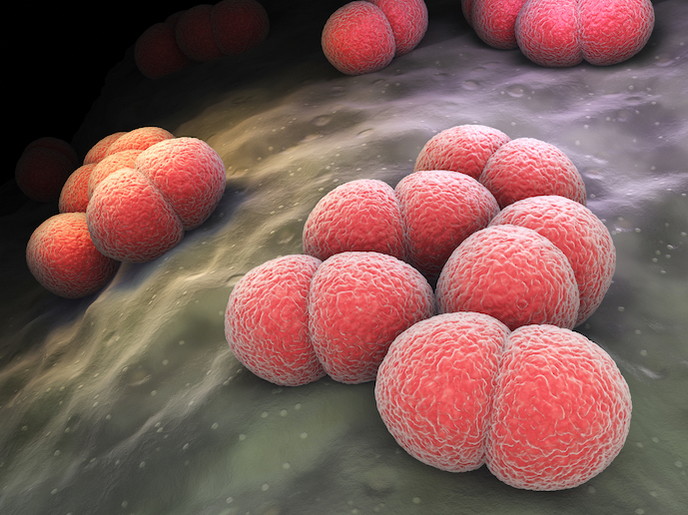
Inflammation of the membranes (meninges) and/or cerebrospinal fluid (CSF) surrounding and protecting the brain and spinal cord is a highly contagious and life-threatening illness requiring fast diagnosis and prompt treatment. Neisseria meningitidis (Nm) is an encapsulated bacteria(opens in new window) which causes meningococcal disease (MD) that manifests as meningitis. Over 1.2 million cases of meningococcal meningitis are estimated to occur worldwide each year, resulting in around 135 000 deaths. This organism is a respiratory pathogen that can be spread from person to person by close contact, affecting mainly children (under 5) and young adults. According to the World Health Organization (WHO), even when diagnosed and treated early, 8-15 % of patients die within 48 hours of the onset of symptoms(opens in new window). Without treatment, fatalities can be as high as 50 %, with one in five survivors left with permanent damage such as hearing loss or neurological disability. Given the lethality of the disease, WHO guidelines recommend the development of point-of-care (PoC) diagnostic tests for rapid aetiological diagnosis. The EU-supported MeningoSpeed project met this need by diagnosing MD in less than 15 minutes by detecting Nm in urine samples.
The non-invasive, accurate, rapid and cost-competitive test
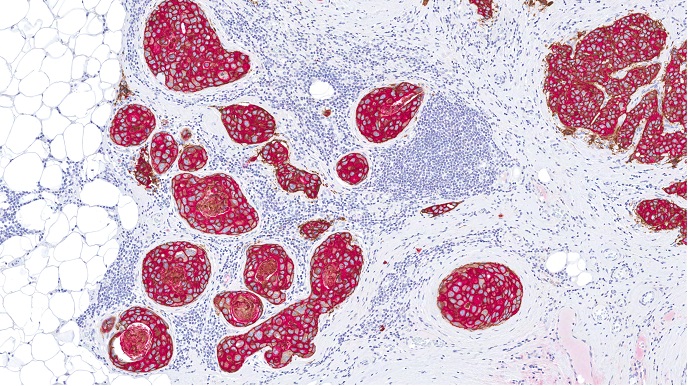
Nm is classified into 12 serogroups(opens in new window), 6 of them (A, B, C, W, X and Y) recognised as the major disease-causing strains capable of generating large epidemics of meningitis. The diagnostic method considered as the gold standard for identifying meningitis cases is CSF culture and polymerase chain reaction(opens in new window) (PCR). However, cultures typically take 48-72 hours for the organism to grow and up to a week for identification, a serious delay for a potentially fatal disease. Meanwhile PCR-based methods require specific laboratory equipment and trained staff and cannot be used as a bedside method. Both methods also require specific laboratory settings, with expensive sample preservation and transportation costs. BioSpeedia(opens in new window) (a spin-off from the Institute Pasteur, France and the project’s hosting institute) had previously developed MeningoSpeed for CSF. The test was clinically validated using 550 CSF samples from six different locations: Central African Republic – IP Bangui(opens in new window), France – University-Hospital of Saint-Etienne(opens in new window), Ivory Coast – IP Abidjan, Morocco – IP Casablanca(opens in new window), Niger – CERMES(opens in new window) and Togo – Agence de Médecine Préventive. The results showed an accuracy rate of 94.9 % (sensitivity and specificity more than 93 %). As project coordinator Yves Germani from BioSpeedia adds: “As the traditional approaches and the original MeningoSpeed using CSF are invasive, they are not practical to use at patients’ bedsides, which is what makes the MeningoSpeed URINE PoC solution extremely valuable.”
The urine test
The MeningoSpeed URINE test consists of three duplex dipsticks which together identify the six serogroups of Nm. The test is a lateral flow immunochromatographic assay(opens in new window) based on direct urine detection of Nm antigens responsible for infection. Crucially, the system can be used by healthcare workers without special training. With encouraging preliminary urine-derived data, the team is working towards conducting a clinical study in hospitals and healthcare centres in France and Africa, with results to be benchmarked against the gold standard PCR method. “The plan is to introduce it globally in 2021 to hospitals, emergency rooms, clinics everywhere, from patient bedside to rural dispensaries,” says Germani. By rapidly diagnosing meningitis, MeningoSpeed and MeningoSpeed URINE will help patients receive the most effective treatment faster, improving health outcomes, as well as reducing illness length, hospitalisations and potential long-term effects. The healthcare system will also benefit as this cheaper diagnostic tool supports rapid epidemic control, leading to significant economic savings.