Novel IBD therapy targets rogue immune cells
Inflammatory bowel disease (IBD) is a debilitating condition where the immune system attacks the gut. It affects 3 million people across Europe(opens in new window), with direct healthcare costs of more than EUR 5.6 billion(opens in new window). The EU-funded LeukoTheranostics project designed a proof of concept treatment for IBD by doping lipid nanoparticles with extraordinarily specific proteins that target only the immune cells that are actively causing inflammation. “This approach gives you fine-tuning of a targeted treatment with much less adverse effect, and the ability to both monitor disease and manipulate specific cells within the immune system,” says project researcher Dan Peer, director of the Laboratory of Precision NanoMedicine at Tel Aviv University(opens in new window).
Preventative action
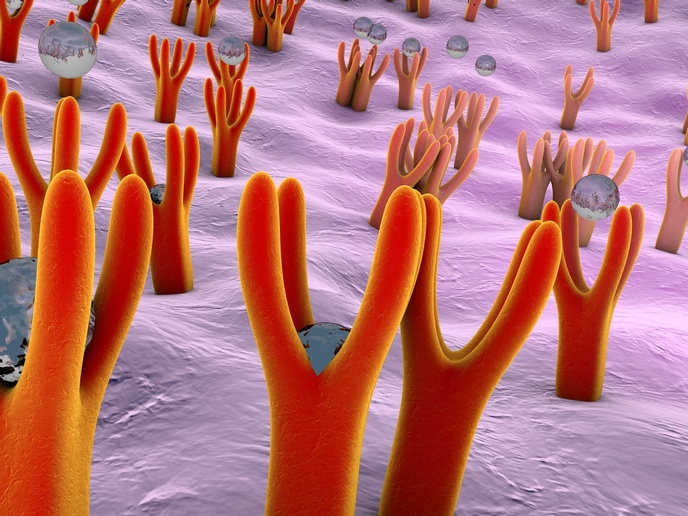
During flare-ups of IBD, leukocytes throughout the body travel to the gut and release cytokines, triggering local inflammation. “Their surface proteins change from a passive to an active conformation, which is a very dramatic structural shift,” explains Peer. Working in mice, his team showed that these activated cells, making up a sixth of the total population, can be targeted through a conformational shift of the a4b7 integrin protein, offering a level of specificity that has never been achieved before. Once the lipid nanoparticles arrive at the leukocytes, they can deliver a therapeutic treatment such as an mRNA gene therapy that deactivates the homing action of the leukocyte and interrupts the release of cytokines. This then subdues the dysfunctional immune response. The specificity of this system means leukocytes not involved in the inflammation will not be affected by the treatment, reducing the necessary dose as well as any side effects.
Tracking disease
The LeukoTheranostics project also showed that by attaching a radionucleotide to the surface of the lipid nanoparticle, they could monitor disease progress using a miniaturised PET/CT scanner. Not only did this make the immune response directly visible – showing where activated leukocytes were congregating – it also allowed them to see the treatment being delivered in real time. Translated into the clinic, this would make doctors less reliant on invasive diagnostic tools such as colonoscopies, which are uncomfortable for the patient as well as expensive and time-consuming to perform. Peer’s lab previously demonstrated that lipid nanoparticles could be used to deliver mRNA gene therapies, a technique which is now being used by pharmaceutical companies to create vaccines for COVID-19. Their work on LeukoTheranostics was supported by the European Research Council(opens in new window). “The ERC grant is a very important resource because this is very expensive research,” he notes. “We have a sophisticated system, in terms of both the lipids we synthesised and the antibodies we generated, which need a very expensive set of skills.” He says the funding made it possible to hire qualified staff, and obtain imaging equipment such as the micro-PET/CT scanner, a first for Tel Aviv University. Peer and his team are now planning to advance their IBD nanoparticle treatment to clinical trials, and he says that the system could also be used to treat other conditions such as cancer: “Everything we have used to monitor the immune status shows that this seems to be a safe treatment system.”