Severe meningococcal infections: is it just the bacteria?
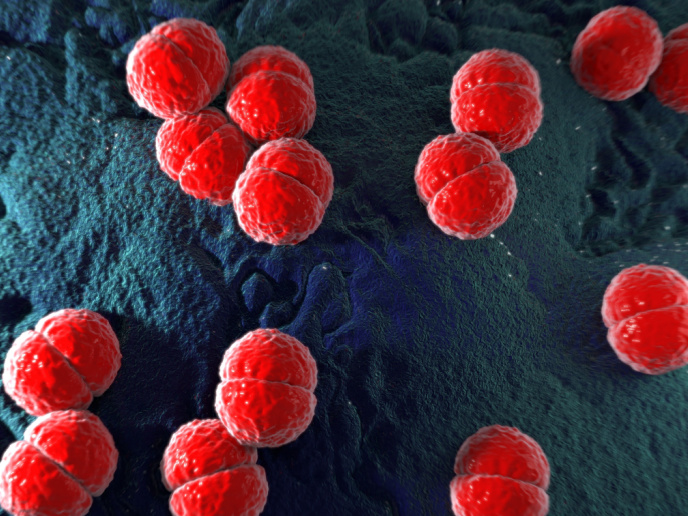
The Gram-negative bacterium Neisseria meningitidis is human-restricted and usually harmless. On rare occasions it can lead to invasive meningococcal disease (IMD), an acute infection that causes swelling of tissues surrounding the brain or bloodstream infection. It must be promptly treated with antibiotics to avoid life-threatening complications. The most recent outbreak of IMD in Europe was reported to have a high mortality and was caused by meningococci of the serogroup W clonal type cc11. Certain immune-related factors such as complement(opens in new window) deficiency predispose individuals to IMD. However, it remains unclear which bacterial, or host factors determine infection progression.
Modelling the stages of meningococcal infection and disease
The EU-funded Eplg Men(opens in new window) project wanted to know why mainly specific meningococcal bacteria cause IMD. The resulting research was undertaken with the support of the Marie Skłodowska-Curie Actions(opens in new window) (MSCA) programme. “There are several steps from exposure to meningococcal bacteria to developing disease and our goal was to model the early stage of colonisation as well as the later invasive stages of severe disease,” explains the MSCA research fellow Gerco den Hartog. The mucosal membrane of the respiratory tract serves as the first barrier against N. meningitidis invasion. If bacteria pass this barrier, then the complement system gets activated to eliminate invading bacteria. The complement system plays an important role in the defence against invading pathogens by generating pores on the bacteria cell wall and then destroying them. Nonetheless, N. meningitidis has acquired mechanisms to evade complement-mediated killing. Researchers selected meningococcal bacteria that caused severe disease in patients and meningococcal bacteria from individuals without any symptoms. Using epithelial cells from the nose as an in vitro model of infection, they compared the infection potential of the different meningococcal isolates. They measured different parameters including the loss of the physical barrier function and the production of cytokines that indicate activation of the immune system. Moreover, incubation of bacterial isolates with serum of unvaccinated and vaccinated people gave an assessment of their resistance to the complement system.
The role of the immune system in meningococcal disease
The in vitro experiments showed that epithelial cells could sense all meningococcal isolates, yet these differed in their efficiency to colonise the human upper respiratory tract. According to den Hartog, “the observed variation in individual responses suggests that it’s not only the bacterium but also the interaction with the host influences bacterial clearance and therefore the risk for disease development.” When they compared the levels of meningococcal-specific antibodies in different age groups they found that children had low levels of antibodies against bacterial proteins. These levels peaked in adolescence and declined with increasing age. By contrast, vaccination generated antibodies against the polysaccharide capsule of bacteria. Meningococcal clinical isolates(opens in new window) demonstrated higher resistance to complement-mediated killing compared with isolates from asymptomatic individuals. Importantly, antibodies induced by vaccination were able to overcome complement resistance and kill all disease-causing meningococcal isolates. Collectively, the Eplg Men work highlights the importance of vaccination for protection during IMD outbreaks and suggests that the currently used MenACWY vaccine protects even against the most resistant meningococcal bacteria isolated from patients.