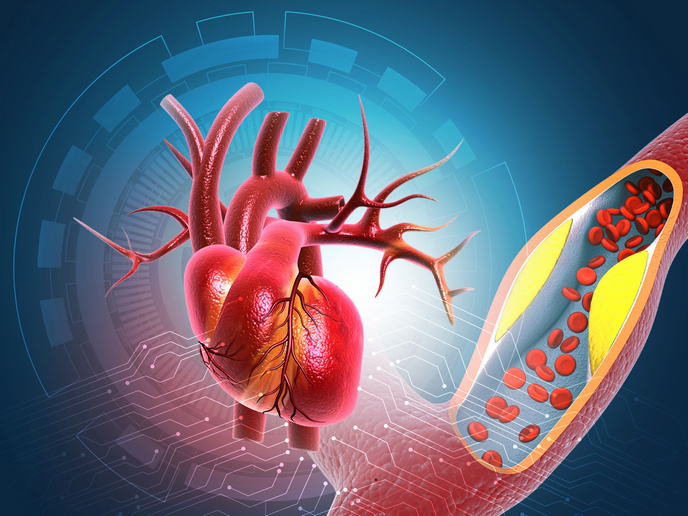
Developing individualised treatment for hypercholesterolaemia
Statins are among the most prescribed drugs in the world. They are an essential treatment for millions of people dealing with hypercholesterolaemia(opens in new window) and are used to reduce the risk of death from heart and blood vessel diseases. The efficacy of statins varies among patients, however. Most patients show good response to the drugs, yet for a significant proportion they either work poorly or not at all. Some patients also experience unwanted adverse effects, such as muscle symptoms. All these factors lead to a notable lack of adherence to statins as a long-term treatment. “Many factors, including genetic variability, diet, other medications and diseases as well as the sex of the patient, can influence both the cholesterol-lowering efficacy and safety of statins,” explains Mikko Niemi(opens in new window), professor in Pharmacogenetics at the University of Helsinki and IndiviStat project principal investigator. “Importantly, there are differences in how the body handles different statins, and this forms the basis for individualising statin therapy,” he adds. The IndiviStat project, which was funded by the European Research Council(opens in new window), developed a systems pharmacology(opens in new window) model to predict statin efficacy and tolerability at the level of an individual patient, and is investigating whether drug selection based on the model improves performance and adherence to the medicines.
Building a systems pharmacology model
The IndiviStat team built a computational model that describes how the body handles the different statins, how the statins inhibit the production of cholesterol in the liver, and how they contribute to problematic effects on the musculoskeletal system. To predict these impacts, the team entered various patient characteristics into the model, such as genetic variants, age, sex, body size, other diseases and medications. They then used the model to simulate the responses to different statins at different doses. First though, the team needed to produce comparative data on the characteristics of different statins themselves. Using cellular and other in vitro models, the researchers compared how the cells handle statins, and explored how genetic variants and other medications affect statin exposures in healthy volunteers. To test their model in a real-world setting, the team carried out an observational clinical trial in patients starting statin therapy and investigated the genetics of statin response in a biobank study(opens in new window). “All these data as well as data from the scientific literature have been used to build and validate our systems pharmacology model,” Niemi explains.
Uncovering individual responses
The results of the project not only showed that statins do differ in their characteristics, but also revealed that the differences in how patients’ bodies handle the drugs are a key driving force behind individual responses. “The most important result from the project is the systems pharmacology model, which is yet to be published,” notes Niemi. IndiviStat is the first project to use predictions from systems pharmacology to guide clinical drug therapy. The team will run a trial using their model as a decision support tool in selecting cholesterol-lowering medication, based on the risk of adverse effects and adherence to statin therapy. The team also plans to use their model to feed into other pharmaceutical development. “If the model proves to be useful in the clinical setting, we will be exploring a similar approach in other fields of drug therapy,” says Niemi.