Personalised approach for liver disease
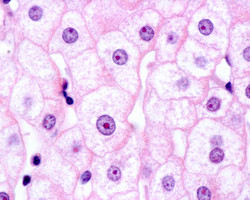
As the main organ of detoxification, the liver is implicated in many diseases and the only effective treatment is liver transplantation. However, the availability of donor grafts is limited and the technique brings about post-surgery complications. Accumulating evidence indicates that transplantation of donor hepatocytes may be sufficient to restore liver function. To exploit this method, technical difficulties in culturing and cryopreserving hepatocytes need to be overcome. The scientists of the EU-funded INNOVALIV(opens in new window) (Innovative strategies to generate human hepatocytes for treatment of metabolic Liver diseases: Tools for personalized cell therapy) study looked into human embryonic stem cells (hESCs) and human induced pluripotent stem cells (hiPSCs) as sources of hepatocytes. INNOVALIV has developed scale-up conditions for undifferentiated VAL9 cells and other pluripotent stem cells and a master differentiation protocol. In addition, other protocols have been defined to differentiate VAL9 cells into functional hepatocytes. These conditions also enable differentiation of other PSCs. Cells derived from two of these protocols have been validated in vivo for safety issues and for cell functions. They were able to proliferate after engraftment and rescued mice with acute failure with no evidence of tumorigenicity. Conditions for large-scale production of hESCs in suspension that are compliant with good manufacturing practice have also been defined. For a personalised cell therapy approach, hiPSCs have been generated from familial hypercholesterolaemia, haemophilia B and Crigler–Najjar liver diseases. The stem cells were then expanded, cryopreserved and differentiated into hepatocytes. A pioneering approach involving targeted recombination was developed to correct mutated genes. The corrected clones expressed the relevant protein and assumed a new phenotype. A rat model showed long-term correction of hyperbilirubinaemia with no evidence of tumour development. Ongoing evaluation of the characteristics and function of these cells will determine their applicability in a clinical setting. A preclinical dossier has been prepared for safety and quality control standards in readiness for the application of the new protocol to clinical trials. Successful cell-based therapy for liver diseases will obviate the need for transplant and a life-long need for immunosuppressive drugs.