Personalised ‘living implants’ offer hope for osteoarthritis sufferers
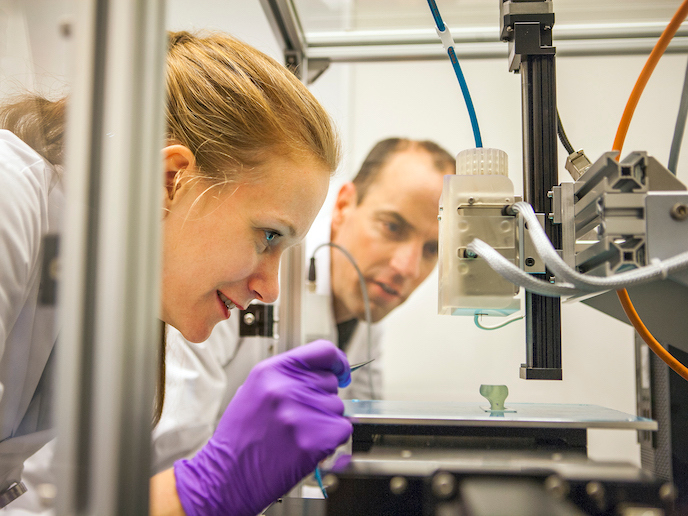
Joint damage causes pain and loss of function, often impairing mobility. It can also trigger a vicious cycle of increasing degeneration of the cartilage and bone underlying joints, leading to the disabling disease of osteoarthritis(opens in new window) (OA). OA is the leading cause of frailty among the elderly, occurring in over 40 million people in Europe(opens in new window). With our rapidly ageing society, this prevalence is set to dramatically rise, increasing the associated healthcare costs. The 3D-JOINT project, supported by the European Research Council(opens in new window), developed personalised ‘living implants’ from simultaneously 3D-bioprinted resorbable thermoplastic polymer filaments(opens in new window) and cell-laden hydrogels(opens in new window) to promote joint regeneration. “Depositing biomaterials and cells layer-by-layer allowed control over their placement and organisation. This precision resulted in durable tissue with much better biomechanical properties,” explains Jos Malda, project coordinator. “Technology to fabricate implants this way had not been developed before.”
Advancing state of the art
Transplanting specialist cells is a better solution than simply repairing diseased or damaged tissues, as it allows these cells to aid in natural joint regeneration. The use of donor stem cells, as a single step approach, has been explored before. However, transplantations have not created stable enough implants, nor adequately matched the contours of the joint. 3D-JOINT’s bioprinting approach was able to meet both criteria. To treat cartilage defects, cells are harvested from patients, multiplied in the laboratory, then implanted back into the defective area, keeping them in place using a soft matrix and/or fibrin glue. Firstly, to validate the biofabrication approach and to assess the mechanical integrity of the implants, cylindrical composite constructs were developed. These contained integrated bone and cartilage printed from biomaterials and cells. For subsequent generations, the constructs were scaled up, and more intricately shaped implants were made. 3D-JOINT’s converged bioprinting process improved the integration of cartilage and bone components, while enabling control over the simultaneous deposition of microfibres and cells. The microfibres added to the structural integrity of the implant as they were fused into a calcium phosphate-based upper cartilage part and a lower bone part, in which these fibres are anchored. This ensured the integration of the two parts. The hydrogel polymers provided an ideal scaffold for new cartilage formation with the regenerative cells deposited across a tissue-specific matrix throughout the gel. “Computational models and advances in microfibre design, inspired by the orientation of collagen fibres in native tissue, significantly increased both the compressive and shear properties of these implants,” reports Malda. Testing their approach in equine models, the team improved the design of micro-scale plug implants used to treat osteochondral injury(opens in new window), and these were shown to withstand the challenging environment of the stifle joint(opens in new window). Following this, larger personalised osteochondral constructions, based on CT scans and consisting of a fibre reinforced cartilage layer, were fabricated and mechanically tested in an ex vivo goat model.
Knowledge-sharing for future developments
Knowledge acquired during 3D-JOINT has already been introduced to the next generation of researchers through the Utrecht University Biofabrication Master’s programme(opens in new window), a yearly summer school(opens in new window) and an E-course. Through BioArchitect(opens in new window), a Eurostars(opens in new window) project, 3D-JOINT has also helped REGENHU(opens in new window), a world-leading manufacturer of high-end bioprinting equipment, to develop a commercial converged bioprinting system. “We are now focused on developing our flexible bone-inducing biomaterial as a durable treatment for hip dysplasia,” says Malda. As for the repair of larger cartilage defects, the team are preparing a larger equine clinical study, before looking to start human trials.