Brain immune system cross-talk in acute neurodegeneration
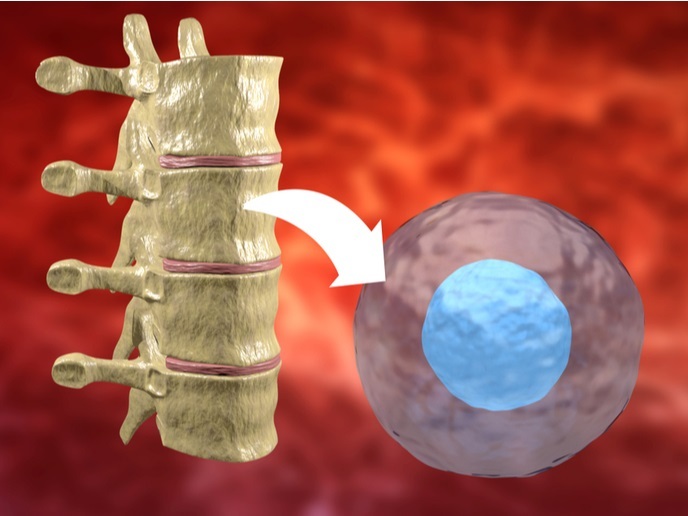
During a sudden insult of ischaemic stroke, neurons rapidly die but additional cellular loss can occur hours and days thereafter, with limited repair. The brain responds by activating resident cells such as microglia and astrocytes and producing pro-inflammatory mediators that attract various types of immune cells. Administration of anti-inflammatory treatments in acute and chronic neurodegenerative diseases has largely been unsuccessful. This possibly reflects the heterogeneity of the immune response, the implicated mechanisms and the importance of the time of administration post-injury. To shed light into the events after stroke, the EU-funded TARGETBRAIN (Targeting brain inflammation for improved functional recovery in acute neurodegenerative disorders) project investigated the role of inflammation and in particular, the cross talk between the brain and the immune system. Activities focused on understanding cell renewal and functional plasticity following an acute neurodegenerative event. The ultimate goal was to create the basis for a novel immunomodulatory therapeutic strategy after stroke. Researchers found that bone marrow monocytes respond to pro-inflammatory cytokines secreted after stroke and enter the brain through the choroid plexus epithelium. These cells were responsible for post-stroke recovery. Microglia and astrocytes were analysed with respect to their fate following an ischaemic episode. The team identified a central role for complement C3a in avoiding astrocyte-mediated brain tissue loss and cognitive impairment. Furthermore, they showed that neural stem cells can act beyond cell replacement and participate in local and systemic immunomodulation. The consortium discovered that delivery of monocytes improved recovery following acute damage to the central nervous system, while a new drug candidate was developed against the inflammatory response. Overall, the TARGETBRAIN project underscored the potential of immune system targeting and stimulating the brain’s own capacity for self-repair in stroke treatment. Considering the millions of individuals who have suffered stroke, the findings of the study have broad socioeconomic implications.