Biobank innovation could lead to targeted leukaemia treatments
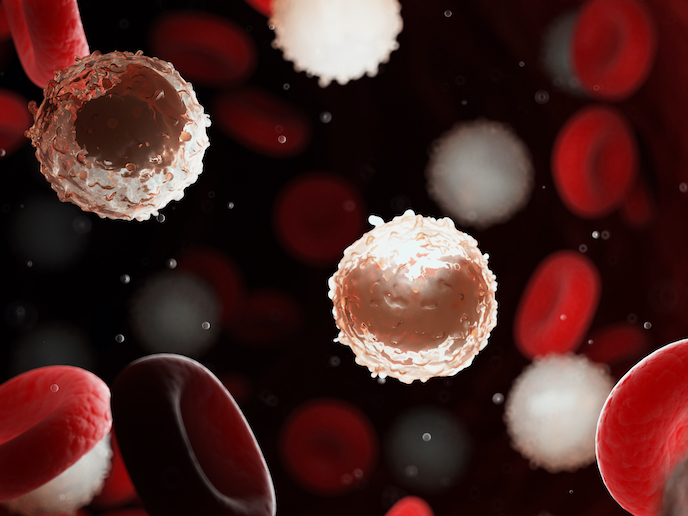
Acute myeloid leukaemia (AML)(opens in new window) is a disease where white blood cells proliferate uncontrolled and displace red blood cells and platelets. This can lead to fatigue, bleeding and a high risk of acquiring infections. “Despite our increased understanding of the underlying mechanisms, current treatments can only cure between 40 and 50 % of younger patients and 10 to 20 % of older patients,” says PNANOMED(opens in new window) project coordinator Michael Heuser, a clinician-scientist at Hannover Medical School(opens in new window) in Germany. A key challenge to treating this condition is the fact that few patients are alike. Even within a single patient, leukaemic cells vary enormously, and many of these cells do not respond to treatment. The difficulty of developing clinical models that represent this complexity has been an obstacle to achieving breakthrough research.
Innovations in screening
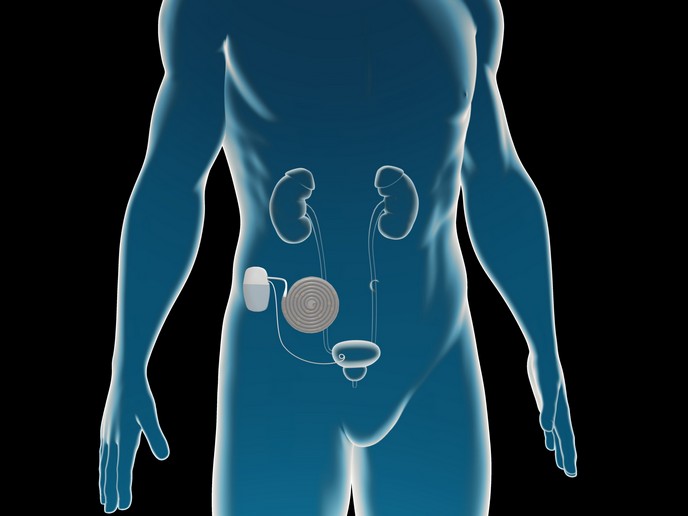
To address this challenge, the PNANOMED project, which was undertaken within the Marie Skłodowska-Curie Actions programme(opens in new window), was launched with several key objectives in mind. Heuser wanted to establish a genetically characterised biobank of AML xenografts(opens in new window) (tissues that can be transplanted from one species to another, in this case, humans to mice). He then sought to characterise the mutations in these xenograft models, and from this, identify effective strategies capable of stopping the tumour-causing activity of these mutated genes. “This biobank of human AML cells was transplanted into immunodeficient mice,” he explains. “Our ability to serially transplant these patient-derived leukaemia cells enabled us to screen therapeutics targeting leukaemia-related mutated genes.” Through this technique, Heuser and his team discovered that combining azacitidine(opens in new window) (a drug that switches on genes that stop cancer cells growing and dividing) and another anticancer drug called trametinib(opens in new window) significantly prolonged the survival of mice, compared to single-agent treatments. The project team was also able to develop a highly efficient and non-toxic nanoparticle-based delivery system for small RNA(opens in new window) pieces (siRNA) that shut down the activity of cancer-causing genes. The delivery system is similar to the ones currently being developed for mRNA SARS-CoV-2(opens in new window) vaccines and Heuser expects that the broader use of this technology will also benefit cancer patients.