A first for the treatment of pancreatic cancer in mouse models
Despite being one of the leading causes of death worldwide(opens in new window), most cancers are treatable if detected early enough. Pancreatic and lung cancers, however, are noteworthy for their low survival rates. “These cancers usually only cause symptoms when well-advanced, making surgical tumour removal or other treatments, very difficult,” says Mariano Barbacid, project coordinator of the THERACAN project, which was funded by the European Research Council(opens in new window). As both cancers are driven by specific genetic mutations, known as KRAS oncogenes(opens in new window), THERACAN used genetically engineered mouse (GEM) tumour models (in vivo and in vitro), to investigate the underlying molecular mechanisms responsible. The project identified new therapeutic targets involved in KRAS oncogenic signalling, demonstrating that the tumour cells regressed in both cancers after these targets were eliminated by genetic manipulation.
The role of KRAS oncogenes
According to Barbacid, KRAS oncogenes are responsible for about a quarter of all solid human tumours, including 25 % of lung adenocarcinomas(opens in new window) (cancers which start in the glands lining organs) and more than 90 % of pancreatic tumours. Despite being among the first human oncogenes discovered, back in 1982, it had been thought that, due to their size and shape, KRAS oncoproteins could not be targeted by drugs. Only recently have pharma companies been able to design KRAS oncogene selective inhibitor drugs. Yet, as Barbacid explains, options remain limited. “So far, the United States Food and Drug Administration(opens in new window) has only approved two inhibitor drugs for one of the KRAS mutated forms. Unfortunately, clinical results have been modest with only half of lung cancer patients experiencing tumour regression. The lung cancer survival rate at two years was the same as that observed with old cytotoxic treatments. The results were even less impressive in pancreatic tumours, making it urgent that we develop new inhibitors.”
Genetically engineered mice
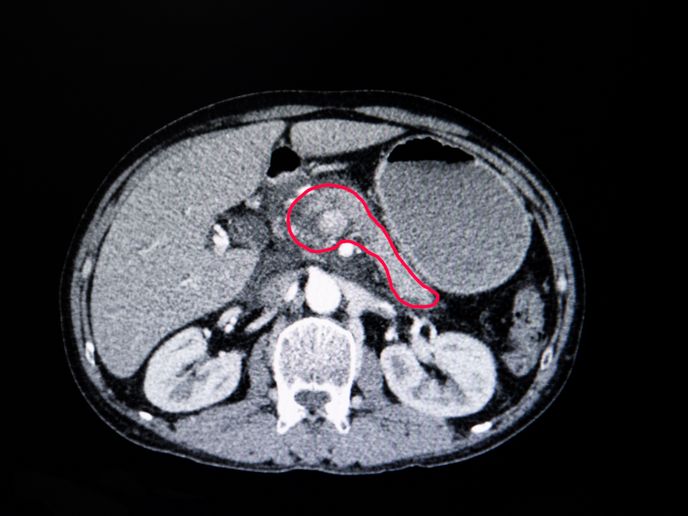
GEM tumour models allowed the team to delete the oncogene protein targets suspected of playing an important role in tumour development. The team showed that eliminating RAF1, a protein involved in KRAS signalling (which controls cell proliferation, including of cancers), led to the regression of two thirds of KRAS mutant lung tumours. Even more importantly, eliminating both RAF1 and the EGF Receptor (also part of the signalling process), resulted in the complete regression of a high percentage of pancreatic ductal adenocarcinomas. As there are no selective RAF1 inhibitors that could be used to validate results, the team did so in patient-derived xenograft(opens in new window) tumour models (human tumour cells grown in mice). Whereas the cancer drug, Gefitinib(opens in new window), was used as an EGFR inhibitor. “This was the first report(opens in new window) of the complete regression of this tumour type in any experimental model,” notes Barbacid. “Even though we demonstrated this in an animal model – so, not directly comparable to humans – observing the complete disappearance of pancreatic tumours was hugely exciting.”
Speeding up the availability of new therapies
As pharmaceutical treatments typically take many years to progress from clinical trials to medical practice, projects such as THERACAN play a vital role in identifying promising targets for therapeutic intervention. “Our work helps the pharma industry focus its resources, speeding up the time it takes to develop the selective inhibitor drugs, ultimately benefiting cancer patients,” concludes Barbacid. The team is now pursuing an EU-funded project to develop new genetic strategies to completely regress all KRAS mutant lung and pancreatic tumours in GEM models.