Understanding the mysterious cell bodies that help cure leukaemia
Acute forms of leukaemia can progress quickly and aggressively. In these cases, abnormal white blood cells multiply rapidly, enter the bloodstream and crowd out healthy blood cells, with the condition demanding immediate treatment. The good news is that the genetics of leukaemia are more understandable to scientists than those of solid tumours. This has led to the development of numerous targeted therapeutic options in addition to chemotherapy and stem cell transplants. “From our understanding of disease pathogenesis, we can optimise existing therapies,” explains PML-THERAPY(opens in new window) project coordinator Hugues de Thé from France’s National Institute of Health and Medical Research(opens in new window) (Inserm). “In particular, my research group is interested in identifying the cellular and biological bases for how these cancers respond to treatments.”
Therapeutic responses of acute myeloid leukaemia
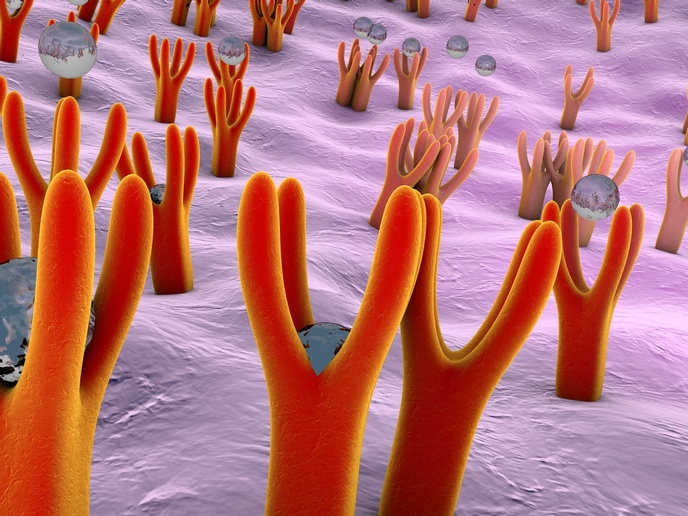
In the PML-THERAPY project, funded by the European Research Council(opens in new window) (ERC), de Thé and his team are focusing specifically on the therapeutic responses of acute myeloid leukaemia (AML). Broadly speaking, AML is an aggressive form of leukaemia that targets the monocyte or granulocyte cells. The project builds on the findings of STEMAPL, a previous project funded by the ERC which successfully identified the molecular basis for therapeutic responses to a specific form of AML called acute promyelocytic leukaemia (APL). “Here, we were able to unravel the mechanisms underlying these cures, and our findings were subsequently validated in patients,” says de Thé. “Targeted therapies now allow us to cure virtually all APL patients.” A key feature of the validated APL cures was their ability to activate promyelocytic leukaemia (PML) nuclear bodies. These subnuclear structures, 0.1 to 1.0 micrometres in diameter, are found in most cell lines and many tissues, but many aspects of their purpose and function remain unclear. “The primary objective of our current ERC project is to decipher whether PML nuclear bodies play any role in the response of other forms of leukaemia to therapy,” explains de Thé.
Evidence implicating PML nuclear bodies
To achieve these aims, the project combined basic biochemistry, cell biology and experimental therapeutics. Mice models were developed to help the team compare therapeutic responses in settings where PML nuclear bodies could no longer form. “These mysterious nuclear domains have fascinated cell biologists for years, and still remain quite a challenge,” adds de Thé. In particular, the project team investigated therapeutic reactions in two conditions. These were myeloproliferative neoplasms (in which the bone marrow produces too many red blood cells, white blood cells, or platelets) and AML with mutations in the gene NPM1c. “Without going into too much technical detail, we found evidence that implicates PML nuclear bodies in therapy response in both conditions,” notes de Thé. “From this knowledge, we have been able to elaborate, in mice models, new therapeutic approaches based on novel drug combinations.”
New treatments and drug combinations
Unravelling the molecular mechanisms associated with therapeutic responses will help to foster new treatments, notably novel drug combinations. The development of such effective, non-invasive therapies will bring clear benefits to cancer patients, and save healthcare systems money by transitioning treatments from long-term care towards cures. “Our studies imply a much broader role for PML in therapy response than was initially anticipated,” remarks de Thé. “This justifies the emphasis we have put on PML biology, as it may yield further therapeutic approaches.” The PML-THERAPY project runs until March 2024, and discussions are currently ongoing regarding the possibility of clinical trials. “I am confident these will happen, because the biological rationale is very strong,” says de Thé.