Unravelling the connection between fat cells, inflammation and the microbiome
In 2022 almost 60 % of adults and nearly one in three children were overweight or obese in Europe, notes the World Health Organization(opens in new window). As the trend is showing no sign of a downturn, improving our understanding of the relationship between the changes adipose tissue undergoes in obesity, and the impact that might have on inflammation is timely. “In the last two decades we have recognised that the relationship between the functions and interactions of our immune cells and white fat cells, adipocytes, are critically important to our health,” says Eran Elinav(opens in new window), professor in the Department of Systems Immunology at the Weizmann Institute of Science(opens in new window) and director of the Microbiome and Cancer Division at the German Cancer Research Center(opens in new window) (DKFZ). Elinav, who coordinated the European Research Council(opens in new window) (ERC) supported ADIMMUNE project, explains that the precise molecular nature of such interactions, such as the types of cell subsets signalling to each other, and the nature of those signals, remain unknown in most cases. “This is due to both methodological and conceptual reasons. For example, the technology that allows us to characterise the gene expression profiles of single cells, known as single cell transcriptomics, has only recently been developed. But the process is challenged by fat cells, which have particular traits.” Even more demanding is unravelling the impact that the large communities of microbes residing within our bodies, our microbiome, have on the networks of communication between our cells, the tissue dynamics and the concomitant effect on our health. “In our project, we set out to meet all of these challenges, by functionally decoding the cell interaction networks in adipose tissue, their molecular nature and their regulation by the gut microbiome,” adds Elinav, who heads the ElinavLab(opens in new window).
Comprehensive analytical tools
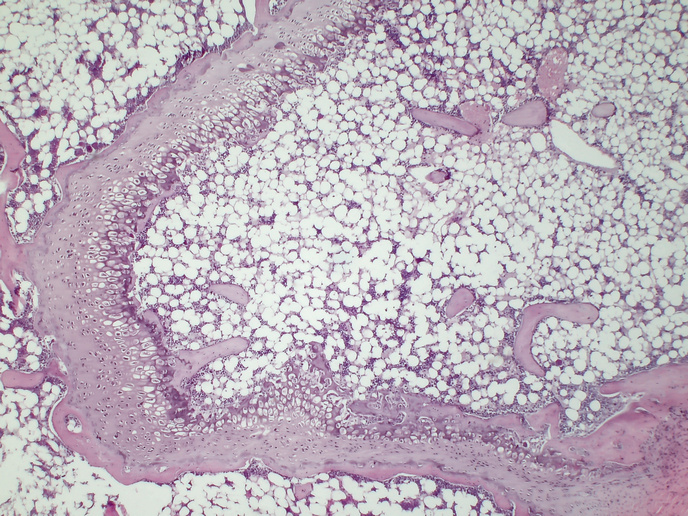
The project used recently developed, high-throughput, (rapidly generated) genomic, microbiological and gnotobiotic(opens in new window) tools, in newly generated mouse models. Gnotobiotic refers to the fact that the mice models were germ-free and then colonised with specific strains of bacteria. The result being that the team was able to precisely identify which bacteria were provoking any given interaction. Their comprehensive approach also integrated an analysis of how genes of certain bacteria in the gut microbiome were functioning, using CRISPR(opens in new window), microbial culturomics(opens in new window) and in vivo metabolic analysis. For these studies, ADIMMUNE drew on human volunteers, both lean and obese, who underwent fat biopsies.
Understanding interaction at single cell level
“We revealed many hitherto unknown interactions,” adds Elinav. Elinav’s team was able to characterise previously unknown types of immune cells in the fat tissue of the mice strains and in both lean and obese human volunteers. Such in-depth characterisation means the project was able to identify multiple, unknown cell subsets, their respective functions at a single cell level, and the communication networks between different cells. “This enabled us to set out the chain of events in which perturbation of such cellular and gene expression communication networks leads to the development of obesity, insulin resistance and the closely associated liver condition, metabolic dysfunction-associated fatty liver disease,” explains Elinav. His findings on obesity are set out in a paper published in the journal ‘Cell’(opens in new window) while those on fatty liver appear in a paper published in the journal ‘Nature Medicine’(opens in new window). The project also addressed one of the most dramatic forms of obesity, known as ‘smoking cessation-associated weight gain’ (SCWG): the mechanism of this phenomenon had been unknown. In a large series of experiments in mice, the team was able to demonstrate that SCWG is substantially regulated by functional changes occurring in the gut microbiome during active smoking, as explained in another paper in ‘Nature’(opens in new window). “We’ve identified the molecules by which the microbes communicate with the fat cells to induce these obesity effects,” notes Elinav. “Intriguingly, once discovered, the molecules could also impact obesity developing in the non-smoking context.” Another groundbreaking thread of the team’s research investigated the interplay between hyperglycaemia and diabetes, and the increased risk associated with lung viral infections, ranging from influenza to COVID-19. It is estimated that over 35 % of humans suffering severe life-threatening COVID were diabetic. “In a study also published in ‘Nature’ in 2023(opens in new window) we demonstrated, in mice, that this enhanced susceptibility of diabetics to pulmonary viral infection, stems from the high levels of glucose in their blood,” says Elinav. He established that high glucose has an impact on the metabolic circuits of a particular immune cell in the lung, termed CDC1. Ultimately this results in altered function that enables the virus to overcome the immune system and generate severe infection.
Functional insights reveal possible treatment paths
These deep dives into the molecular basis of the communication between the bacteria we host, and the immune cells in our adipose tissue, have resulted in functional insights leading to possible treatment paths. Elinav is proud of the project’s achievements: “Establishing such causative and mechanistic levels of understanding enables the identification of therapeutic targets, and even the molecules that modulate disease development. We couldn’t have done it without the without continued support from the ERC.”