Insights into the mechanisms of cancer-specific immunity
It was long debated whether the immune system, in particular T-cells(opens in new window), can stop human cancer cells from growing. Recent work has shown that in a significant number of human cancers, a T-cell response is indeed initiated, especially in tumours with more DNA damage – making cancer cells appear more ‘foreign’ to the immune system. According to Ton Schumacher(opens in new window), coordinator of the SENSIT project, “The next key questions are: how exactly does this T-cell activity influence tumour cell behaviour and how do tumours respond?” To address these questions, SENSIT, which was funded by the European Research Council(opens in new window), explored the interaction between immune cells and cancer cells in human cancer tissue. “We found that when T-cells are activated they send out signals that alter the tumour tissue in general, over long distances, rather than simply killing only the tumour cells they directly interact with,” explains Schumacher from the Netherlands Cancer Institute / Leiden University(opens in new window), the project host.
Developing exploratory platforms
SENSIT benefited from three complementary approaches geared towards development of new technological platforms. Genetic screening technology was used to identify processes that control the expression of PD-L1 and CD47, two key regulators expressed in tumour tissue that suppress immune cell activity (also known as ‘immune checkpoints’). The team showed that PD-L1’s expression is controlled by a protein called CMTM6, and that techniques to influence CMTM6 could potentially alter the expression of the PD-L1 checkpoint and thereby influence T-cell function. With CD47, its ability to bind its ligand(opens in new window) – so suppressing immune cell activity – was shown to be controlled by an enzyme. This suggests the prospect of suppressing activity of the CD47 immune checkpoint using small molecules that inhibit this enzyme, so boosting immune cell activity. SENSIT also developed and used technology that tracked how the cytokines(opens in new window) that are secreted by T-cells when activated, influence tumour cells adjacent to or further away from the site of T-cell activity. “It had been assumed that cytokines primarily act on the target cell recognised by a T-cell, but we showed that IFNg secretion works as an ‘alarm system’ influencing tumour cell activity over long distances, increasing expression of antigens, making the tumour cells more visible to T-cells,” says Schumacher.
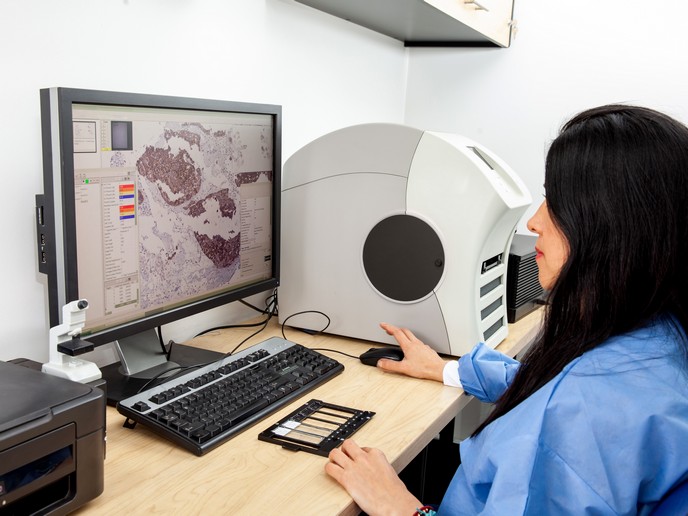
Evaluating immunotherapy
To evaluate how immunotherapeutic interventions influence immune cell activity in human cancer tissue, the team also created an ex vivo human tumour culture platform. Using this platform, the team showed that therapeutic antibodies that block the activity of the immune checkpoint PD-L1, activate immunity in human tumour cultures, correlating with actual clinical patient response. “Contrary to the view that T-cells within the tumour are exhausted, implying that T-cells in lymphoid organs would have to be engaged instead, many of these immunotherapy effects are actually due to T-cell reactivation at the tumour site,” notes Schumacher. “Additionally, we identified a number of immune cell properties that predict the capacity of T-cells in human tumours to be rekindled by inhibiting the PD-L1 checkpoint.”
Helping patient selection
SENSIT’s work could be used to help identify patients most likely to benefit from this immunotherapy, while also offering a starting point to identify more effective cancer treatments for those less likely to respond. “Additionally, our discovery about the rewiring of the tumour microenvironment by cytokine secretion could contribute to the development of more effective immunotherapies,” adds Schumacher. To advance this discovery, Schumacher suggests conducting studies into patient-specific differences in how far these signals reach in tumour tissue and the patient-specific effect of these signals on the tumour tissue.